Abstract
Introduction: Diffuse large B-cell lymphoma (DLCBL) is the most common lymphoid malignancy in the United States. The combination of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) has been shown to be effective and is considered as the standard therapy for DLBCL. However, outcomes remain heterogeneous and hence, more detailed analysis is required to correctly characterize the impact of clinical and socio-demographic factors on DLBCL-specific deaths.
Data: Using Surveillance, Epidemiology, and End Results (SEER)-Medicare database, we identified 11,780 patients with DLBCL who were diagnosed between 2002 and 2009. 9,508 of these patients received at least a single therapy after diagnosis. In addition to treatment regimens, DLBCL histology, stage, presence of B-symptoms, history of anemia, extranodal primary site of involvement, Charlson comorbidity index and performance status were identified from the SEER data. Other predictors of poor survival available in the data were patient age, sex, race, geographic region of residence, marital status, year of diagnosis, and census tract-level characteristics such as urban status and education level, as a measure of socioeconomic status. Since all subjects were Medicare beneficiaries, all patients were older than 65 at diagnosis. The last day of follow-up was December 31, 2011.
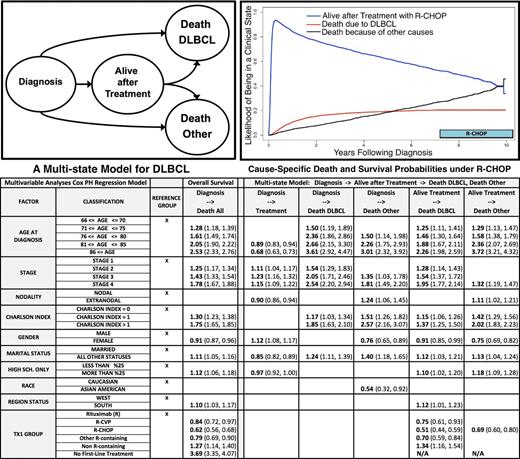
Methods: We developed a multi-state model to study the impact of clinical and socio-demographic factors on DLBCL-specific deaths. Given that senior patients die from many causes, a multi-state model is essential to correctly distinguish deaths due to DLBCL from deaths due to other causes and to identify risk factors affecting DLBCL-caused mortality. The AalenJohansen estimator, a generalization of Kaplan-Meier estimator, was used to estimate the likelihood of being in one of four health states: Alive after diagnosis, Alive after treatment, Dead due to DLBCL and Dead due to other causes (see the diagram, top left). A multivariable Cox proportional hazards regression model was fitted to each transition between the model states to identify significant risk factors affecting the time and rate of each transition. The findings are compared with the findings of the conventional overall survival model to discuss the advantages and necessity of using a more detailed multi-state modeling framework. Percentage of (DLBCL-specific and all cause) deaths within two years and median time to (DLBCL-specific death and overall survival) events are also used to evaluate the impact of identified risk factors.
Results: 5,732 (69% due to DLBCL) and 7,599 (58% due to DLBCL) patients died within 2 years of their diagnosis and before the last day of follow-up, respectively.For patients receiving R-CHOP, the cumulative risk of DLBCL-specific death was exceeded by the cumulative risk of death due to other causes approximately 5.25 years after diagnosis and remained constant afterwards (see the figure, top right). Multivariable Cox regression analyses revealed that higher age, DLBCL stage and Charslon index categories are associated with an elevated risk of DLBCL-specific death both for patients with or without treatment. In addition, being married or female and having higher socioeconomic status are associated with a reduced risk of DLBCL-specific death for patients receiving treatment (see the table attached for the hazard ratios with 95% confidence intervals). As expected, treatment was shown to reduce the risk of DLBCL-specific death, with first-line therapy R-CHOP having the highest positive impact. Consistent with these findings, the factors with higher risk of DLBCL-specific death had lower median time to DLBCL-specific death and median overall survival duration and higher percentage of DLBCL-specific and all cause deaths within two years.
Conclusions: Using a multi-state model, we identified increasing age, DLBCL stage and Charlson comorbidity index, being unmarried or male and low socioeconomic status as significant predictors for overall survival and DLBCL-specific mortality in the elderly population. As opposed to a standard survival model, the multi-state approach enables researchers to capture DLBCL-specific and other deaths separately within the same model and helps accurately examine the influence of factors on each transition.
Flowers: National Institutes Of Health: Research Funding; OptumRx: Consultancy; Onyx: Research Funding; Infinity: Research Funding; Abbvie: Consultancy, Research Funding; Eastern Cooperative Oncology Group: Research Funding; Millennium/Takeda: Research Funding; Bayer: Consultancy; Gilead: Consultancy; Janssen Pharmaceutical: Research Funding; Pharmacyclics LLC, an AbbVie Company: Research Funding; Genentech/Roche: Consultancy, Research Funding; Clinical Care Options: Research Funding; Educational Concepts: Research Funding; Prime Oncology: Research Funding; TG Therapeutics: Research Funding; Acerta: Research Funding; Research to Practice: Research Funding; V Foundation: Research Funding; Burroughs Welcome Fund: Research Funding; Celgene: Consultancy, Research Funding; Seattle Genetics: Consultancy; National Cancer Institute: Research Funding; Spectrum: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal